AIIMS has published the list of candidates who secured 50% or more marks in AIIMS-PG (MD/MS/MCh (6 Years) Entrance Examination, January 2012 Session.
http://www.aiimsexams.org/pdf/50.pdf
A comprehensive question bank for indian medical PG preparations- AIIMS, ALL INDIA, JIPMER, PGI, state exams etc. Visual and audio content prepared in view of upcoming pattern of NEET (National Eligibility & Entrance Test). Best wishes for your preparation! AIPGE content updated with emphasis on recent questions.
How to use this site?
Please click on the comments to see the right option from the choices given
This site contains a comprehensive list of medical PG entrance questions asked in various PG entrance examination throughout India like AIIMS, AIPGEE, PGI CHANDIGARH, JIPMER, CMC VELLORE .... and various state entrance exams like KERALA, TAMIL NADU, KARNATAKA, DELHI .... and also private entrances like COMEDK, MANIPAL etc...
Pages
SEARCH THE WEB
20120131
MMST notification , IIT Kharagpur
School of Medical Science and Technology (SMST), Indian Institute of Technology Kharagpur offers a 3 years post graduate program - Masters in Medical Science and Technology (MMST) for MBBS graduates. This programme imparts engineering skills to medical professionals and train them for the state-of-the-art medical research in frontier areas of Medical Imaging, Molecular Imaging and Image Analysis, Biomaterials and Implants, Biophysics, Medical Statistics, Telemedicine, Biomedical Instrumentation, Early Detection of Cancer, Immuno-technology, Recombinant DNA Technology, Biomedical Simulation, Wound research and so on. After the completion of this course the medical professionals become well equipped to fill the void that separates the medical sciences from advanced technology.
Application Procedure
MMST 2012 application is to be submitted only by an ONLINE process (internet based) by accessing the website http://gate.iitkgp.ac.in/mmst from 23 January 2012 till 9 March 2012. The candidate should first pay the Application Fee by obtaining a Demand Draft drawn in favour of IIT Kharagpur on any nationalised bank payable at Kharagpur, West Bengal. The draft details are require while filling up the ONLINE application form after successful submission of data. The printed form, with candidate's signature and photograph pasted at appropriate place, and the Demand Draft must be sent by speed post so as to reach by 15 March 2012 to The Chairman, GATE, IIT Kharagpur, Kharagpur - 721302.
Following additional documents should be mailed along with the printed Application Form :
1. Attested copy of OBC (Non-creamy)/SC/ST/PD certificate (if applicable)
2. Attested copies of MBBS Degree (recognized by MCI) with mark sheet of all yearsas a proof of obtaining a minimum of 55% marks in aggregate.
3. Attested copy of proof of having studies Mathematics at +2 level (even as an additional subject)
Application Fees
Rs. 1000/- for General Category and Rs. 500/- for SC/ST/PD Category.
FEMALE CANDIDATES ARE NOT REQUIRED TO PAY ANY APPLICATION FEE
Admit Card
Admit Card is issued only to eligible candidates who submit the application form completed in all respects before the closing date. GATE office will dispatch the admit card starting from 3 April 2012. If it is not received by 15th April 2012, the Chairman GATE IIT Kharagpur should be contacted for necessary action. The admit card should be preserved by the candidate even after the examination for the purpose of counseling.
The admission test is of objective type to identify the aptitude of the candidates for a program like MMST. The test is of two hours duration and held between 10:00 A.M.to 12:00 Noon on Sunday, 29 April 2012. The candidate needs to answer 120 questions out of which 75 questions are assigned to the typical MBBS syllabi. The remaining questions are equally distributed to cover the syllabi of +2 level Physics, Chemistry & Mathematics. Each correct answer carries one mark and each wrong answer carries 0.25 negative marks.
Counselling
On the basis of performance in the written test a list of qualified candidates will be prepared and these candidates are called for counseling at IIT Kharagpur on 21 June 2012 (Tentative) before final selection is made for admission.
MANIPAL PG medical test booking starts tomorrow.
PG Medical & Dental - OTBS 2012 will open from February 01, 2012
January 30,2012
Online Test Booking System (OTBS) is a real time web based online scheduling system. The schedule bookings are done on first come first basis and are subject to availability.
Login to OTBS with your application number and password.
In case of non-availability of slots in a centre of choice, the candidate may choose to book a slot in an alternate centre.
A slot once booked cannot be changed. Requests for change of test centre, date and slot will not be entertained under any circumstances.
Click here for the demo on Online Test Booking System .
The Online Test Booking window will be open from February 01, 2012 and will close on February 10, 2012.
Visit www.manipalotbs.com to book the centre, date and time of your choice.
Hurry, book early to before your test centre closes.
NOTE:
Those who have applied online can use password received at that time to book a slot.
If you have not received your password yet, contact manipal at:
0 9243777700admissions@manipal.edu
- If your test centre closes and you haven't yet received a password, you can ask them to book a slot for you after the booking process is over. Keep sending mails to the above id.
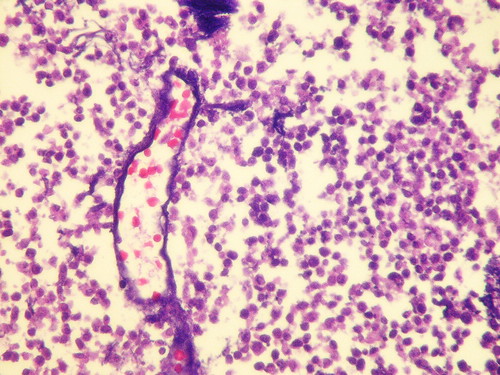
Azzopardi effect:

 In small cell Ca of lung,
In small cell Ca of lung,blood vessels in necrotic area may show smudged hematoxophilic material in their walls, which represents DNA released from tumour cells. This is referred to as Azzopardi effect.
Torus aorticus
The torus aorticus is the prominent region of the right atrial septum
sited superiorly and anteriorly. It is superior to the coronary sinus
and anterior to the fossa ovalis. It represents the deeper and anterior
surface of the posterior sinus and cusp of the aorticvalve.
.

.

omovertebral bone
bony or fibrous connection between scapula and the spinous process,
lamina or transverse process of a vertebral body between C4 and C7.
Seen in cases of Sprengel deformity.
Seen in cases of Sprengel deformity.
PGMCET 2012 answer discussion
Floating Teeth-alveolar bone destruction of part of the mandible from eosinophilic granuloma may make adjacent teeth appear to "float."Also may occur with other destructive lesions of mandible
PGMCET 2012 RECALL- Kauffman White classification
The nomenclature for the genus Salmonella has evolved from the initial one serotype-one species concept proposed by Kauffmann on the basis of the serologic identification of O (somatic) and H (flagellar) antigens. Each serotype was considered a separate species (for example, S. paratyphi A, S. newport, and S. enteritidis); this concept, if used today, would result in 2,463 species of Salmonella. Other taxonomic proposals have been based on the clinical role of a strain, on the biochemical characteristics that divide the serotypes into subgenera, and ultimately, on genomic relatedness.
Salmonella species, subspecies, serotypes, and their usual habitats, Kauffmann-White scheme
| Salmonella species and subspecies | No. of serotypes within subspecies | Usual habitat |
|---|---|---|
| S. enterica subsp.enterica(I) | 1,454 | Warm-blooded animals |
| S. enterica subsp.salamae (II) | 489 | Cold-blooded animals and the environment |
| S. enterica subsp.arizonae (IIIa) | 94 | Cold-blooded animals and the environment |
| S. entericasubsp.diarizonae (IIIb) | 324 | Cold-blooded animals and the environment |
| S. enterica subsp.houtenae(IV) | 70 | Cold-blooded animals and the environment |
| S. enterica subsp. indica(VI) | 12 | Cold-blooded animals and the environment |
| S. bongori(V) | 20 | Cold-blooded animals and the environment |
| Total- 2463 |
PGMCET 2012 review- Schmidt's syndrome
POLYGLANDULAR AUTOIMMUNE SYNDROME'S
When immune dysfunction affects two or more endocrine
glands and other nonendocrine immune disorders are present, the polyglandular
autoimmune (PGA) syndromes should be considered. The PGA syndromes are classified
as two main types:
the type I syndrome starts in childhood and is characterized by
mucocutaneous candidiasis, hypoparathyroidism, and adrenal insufficiency;
the
type II, or Schmidt syndrome is more likely to present in adults and most
commonly includes adrenal insufficiency, thyroiditis, or type 1 diabetes
mellitus. Some authors have attempted to subdivide PGA II on the basis of
association with some autoimmune disorders but not others (i.e., type II and
type III).
The type III syndrome is heterogeneous and may consist of autoimmune
thyroid disease along with a variety of other autoimmune endocrine disorders . However, little information is gained by making this
subdivision in terms of understanding pathogenesis or prevention of future
endocrine complications in individual patients or in the affected
families.
| ||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||
Abbreviation: APECED, autoimmune
polyendocrinopathy-candidiasis-ectodermal
dystrophy.
| ||||||||||||||||||||||||||||||||||||
Polyglandular Autoimmune Syndrome Type I
PGA type I usually is recognized in the first decade of
life and requires two of three components for diagnosis: mucocutaneous
candidiasis, hypoparathyroidism, and adrenal insufficiency. Mucocutaneous
candidiasis and hypoparathyroidism present with similar high frequency (100% and
79–96%, respectively). Adrenal insufficiency is observed in 60–72% of patients.
Mineralocorticoids and glucocorticoids may be lost simultaneously or
sequentially.
PGA type 1 also is called autoimmune
polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED). Other
endocrine defects can include gonadal failure (60% female, 14% male),
hypothyroidism (5%), and destruction of the beta cells of the pancreatic islets
and development of insulin-dependent (type 1) diabetes mellitus (14% lifetime
risk). Additional features include hypoplasia of the dental enamel, nail
dystrophy, tympanic membrane sclerosis, vitiligo, keratopathy, and gastric
parietal cell dysfunction resulting in pernicious anemia (13%). Some patients
develop autoimmune hepatitis (12%), malabsorption (variably attributed to
intestinal lymphangiectasia, bacterial overgrowth, or hypoparathyroidism),
asplenism, achalasia, and cholelithiasis . At the outset, only one
organ may be involved, but the number increases with time so that patients
eventually manifest two to five components of the syndrome.
Most patients initially present with oral candidiasis in
childhood; it is poorly responsive to treatment and relapses
frequently. Chronic hypoparathyroidism usually occurs before adrenal
insufficiency develops. More than 60% of postpubertal women develop premature
hypogonadism. The endocrine components, including adrenal insufficiency and
hypoparathyroidism, may not develop until the fourth decade, making continued
surveillance necessary.
Type I PGA syndrome is not associated with a particular HLA type and
usually is inherited as an autosomal recessive trait. It may occur sporadically.
The responsible gene, designated as either APECED or AIRE, encodes
a transcription factor that is expressed in thymus and lymph nodes; a variety of
different mutations have been reported. The mechanism by which these mutations
lead to the diverse manifestations of type I PGA is unknown.
Polyglandular Autoimmune Syndrome Type II:
PGA type II is characterized by two or more of the
endocrinopathies listed above. Most often these endocrinopathies
include primary adrenal insufficiency, Graves' disease or autoimmune
hypothyroidism, type 1 diabetes mellitus, and primary hypogonadism. Because
adrenal insufficiency is relatively rare, it is used frequently to define the
presence of the syndrome. Among patients with adrenal insufficiency, type 1
diabetes mellitus coexists in 52% and autoimmune thyroid disease occurs in 69%.
However, many patients with antimicrosomal and antithyroglobulin antibodies
never develop abnormalities of thyroid function. Thus, increased antibody titers
alone are poor predictors of future disease. Other associated conditions include
hypophysitis, celiac disease (2–3%), atrophic gastritis, and pernicious anemia
(13%). Vitiligo, which is caused by antibodies against the melanocyte, and
alopecia are less common than in the type I syndrome. Mucocutaneous
candidiasis does not occur. A few patients develop a late-onset, usually
transient hypoparathyroidism caused by antibodies that compete with PTH for
binding to the PTH receptor. Up to 25% of patients with myasthenia gravis and an
even higher percentage who have myasthenia and a thymoma have PGA type II.
The type II syndrome is familial in nature, often transmitted as an
autosomal dominant trait with incomplete penetrance. As in many of the
individual autoimmune endocrinopathies, certain HL-DR3 and -DR4 alleles increase
disease susceptibility; several different genes probably contribute to the
expression of this syndrome.
A variety of autoantibodies are seen in PGA type II,
including antibodies directed against
(1) thyroid antigens such as thyroid
peroxidase, thyroglobulin, and the thyroid-stimulating hormone (TSH) receptor;
(2) adrenal side chain cleavage enzyme, steroid 21-hydroxylase, or ACTH
receptor; and
(3) pancreatic islet glutamic acid decarboxylase or the insulin
receptor, among others.
The roles of cytokines such as interferon and
cell-mediated immunity are unclear.
Diagnosis:
The clinical manifestations of adrenal insufficiency often
develop slowly, may be difficult to detect, and can be fatal if not diagnosed
and treated appropriately. Thus, prospective screening should be performed
routinely in all patients and family members at risk for PGA types I and II. The
most effective screening test for adrenal disease is a cosyntropin stimulation
test . A fasting blood glucose level can be obtained to screen for
hyperglycemia. Additional screening tests should include measurements of TSH,
luteinizing hormone, follicle-stimulating hormone, and, in men, testosterone
levels. In families with suspected type I PGA syndrome, calcium and
phosphorus levels should be measured. These screening studies should be
performed every 1–2 years up to about age 50 in families with PGA type II syndrome and until about
age 40 in patients with type I syndrome. Screening measurements of autoantibodies against
potentially affected endocrine organs are of uncertain prognostic value.
The
differential diagnosis of PGA syndrome should include the
-DiGeorge syndrome
(hypoparathyroidism due to glandular agenesis and mucocutaneous candidiasis)
-Kearns-Sayre syndrome (hypoparathyroidism, primary hypogonadism, type 1
diabetes mellitus, and panhypopituitarism)
-Wolfram's syndrome (congenital
diabetes insipidus and diabetes mellitus)
-IPEX syndrome
(immunodysregulation, polyendocrinopathy, and enteropathy,
X-linked)
-congenital rubella (type 1 diabetes mellitus and
hypothyroidism).
Treatment: Polyglandular Autoimmune Syndrome
With the exception of Graves' disease, the management of
each of the endocrine components of the disease involves hormone replacement. Some aspects of
therapy merit special emphasis.
Primary hypothyroidism can mask adrenal
insufficiency by prolonging the half-life of cortisol; consequently,
administration of thyroid hormone to a patient with unsuspected adrenal
insufficiency can precipitate adrenal crisis. Thus, all patients with
hypothyroidism in the context of PGA syndrome should be screened for adrenal disease and, if it
is present, treated with glucocorticoids before or concurrently with thyroid
hormone therapy.
Hypoglycemia or decreasing insulin requirements in a patient
with diabetes mellitus type 1 may be the earliest symptom of adrenal
insufficiency. Consequently, such patients should be screened for adrenal
disease.
Treatment of mucocutaneous candidiasis with ketoconazole may induce
adrenal insufficiency. This drug also may elevate liver enzymes, making the
diagnosis of autoimmune hepatitis more difficult.
Hypocalcemia in PGA type II is
more commonly due to malabsorption associated with celiac disease than to
hypoparathyroidism.
20120115
General Adaptation Syndrome ( GAS )
When Hans Selye was conducting research on rats by injecting them with extracts of various glands of the body, he noticed that the rats were all displaying the same group of symptoms. At first he believed that he had discovered a new hormone; however, after several years of further testing by injecting the rats with other substances, such as formaldehyde revealed the same results. Even exposure to cold, cutting their spinal cords and forced exercise produced the same effects. The effects occurred in a predictable sequence that is now known as the General Adaptation Syndrome (GAS).
Stage 1 : Alarm
Selye called the first stage of the General Adaptation Syndrome the General Alarm Reaction. This reaction is the result of the biological processes that were described in the section on The Body's Response to stress: Signals are sent to the sympathetic division of the ANS, which increases heart rate, dilates bronchi, inhibits digestion, converts glycogen to glucose etc; meanwhile the hypothalamus also releases CRF, which in turn prompts the release of ACTH from the pituitary which stimulates the secretion of cortisol from the adrenal-cortex.
Stage 2 : Resistance
If the stressor is not removed the body attempts to adapt to the stress and in the second stage, resistance, it is largely successful; nevertheless, adrenaline and cortisol levels remain high. The consequence of this is that although the body is able to cope, its resources are depleted. If the stress continues for longer the third stage of the syndrome is reached.
Stage 3 : Exhaustion
Resistance to stress can only be maintained for a limited amount of time. As the body's resources become depleted, the immune system is weakened and health problems develop.
Japanese detergent poison- AIIMS offering easy way out???
More recently people have been using a new way of bringing their lives to an end. This technique is called ‘detergent suicide’ or ‘chemical suicide’. It involves mixing a number of readily available household chemicals, such as toilet bowl cleaner with other reactive elements to create a poisonous gas such as hydrogen sulphide. Inhaled in small doses, at less than 40 parts per million (ppm), exposure to this gas can cause eye and mucous membrane irritation. But as the dosage level increases people exposed can quickly experience confusion and cyanosis with coughing fits. At dose levels above 500 ppm patients often die. At 700 ppm two or three breaths can cause immediate death.
To achieve high dosage levels the people intent on suicide often either tap up the windows in their houses and attempt to seal a single room or use a car to decrease the volume of air in which the toxic material is released. With hydrogen sulphide being a colourless gas it can be a major hazard for first responders whose first inclination on seeing a body slumped in a car might be to characterise the incident as a methane poisoning and break the car window, accidentally exposing themselves to a much more threatening situation.
To achieve high dosage levels the people intent on suicide often either tap up the windows in their houses and attempt to seal a single room or use a car to decrease the volume of air in which the toxic material is released. With hydrogen sulphide being a colourless gas it can be a major hazard for first responders whose first inclination on seeing a body slumped in a car might be to characterise the incident as a methane poisoning and break the car window, accidentally exposing themselves to a much more threatening situation.
It is not difficult to imagine a small device being carried into a shopping centre in a disguised form by a potential martyr who then mixes the two chemicals in a way that spreads gas over a relatively small area. Whilst the death toll is unlikely to be high the impact upon the public might be considerable. When death comes in the form of a colourless gas it can easily dent public confidence. Even what on the surface appears to be a hugely amateurish attack could still have significant economic repercussions.
For the Fire and Rescue Service some enduring lessons are clear. Dispatchers involved in taking calls need to be alert to the indications that they are sending crews into this kind of situation. Careful questioning of the caller is important with any references to bad odours, such as a smell of almonds (indicative of a cyanide compound) or rotten eggs (indicative of the presence of hydrogen sulphide) needing to be taken seriously.
As responders attend the scene they need to be on the look out for situations where a person may have attempted to create the kind of environment in which dosage levels can quickly reach fatal levels. Residential bathrooms, cars and other small spaces – especially when sealed off from the outside – are all places to be wary. In apartment buildings, as occurred in the incident in Japan referred to earlier, a decision may need to be taken about evacuation. The presence in a vehicle of large tubs or containers is also a major indicator. Relying on the presence of warning signs to provide a strong indicator would also place first responders at risk from a terrorist-related event where the perpetrator is seeking to use the situation to draw first responders into a hazardous situation.
Despite the development of the idea that detergent suicide was a painless and straightforward method for those seeking death, the potential for such techniques to be adapted and used by those involved in terrorism cannot be ignored. Terrorism has a history of developing in unexpected ways and it is important for the members of the Fire and Rescue Service to always be prepared for the unexpected. Whilst it is a well known cliché, it may also ensure that some of them do not accidentally become exposed to fatal levels of a concoction readily assembled from advice over the Internet and a few visits to the supermarket.
TERATOGENIC DRUGS
Women of childbearing age with chronic medical conditions are often concerned about hazards from drug exposure during pregnancy and lactation.
The number of mothers who take drugs during pregnancy is not known, but a U.S. survey showed that about 45% of women may use at least one drug on prescription, and many more use drugs bought over the counter. A British prospective study suggested that only about 10% of women take drugs in early pregnancy.
The avoidance of any medication after conception may often be unwise for maternal well-being. Proper prescribing of drugs in pregnancy is a challenge and should provide maximal safety to the foetus as well as therapeutic benefit to the mother. Double-blind, randomized, prospective drug trials are generally impossible to perform during pregnancy. Certain medical disorders occur infrequently at any one medical centre or cannot be studied during pregnancy for ethical or regulatory reasons.
Major congenital defects occur in 1-3% of the general population at birth. Careful follow-up increases the number detected to up to 5% later in life. Major birth defects cause 20% of infant mortality and are responsible for a substantial number of childhood hospitalizations. Of those defects about 25% are of genetic origin (genetically inherited diseases, new mutations and chromosomal abnormalities) and 65% are of unknown etiology (multifactorial, polygenic, spontaneous errors of development and synergistic interactions of teratogens). Only 2-3% of defects are thought to arise in association with drug treatment. The remaining defects are associated with other environmental exposures during pregnancy including infectious agents, maternal disease states, mechanical problems and irradiation.
Maternal physiologic changes in pregnancy may alter the pharmacokinetics of drugs. There is large variability in maternal metabolism and elimination of drugs during pregnancy. Clearance rates of many drugs increase during late pregnancy due to increases in both hepatic and renal elimination processes (e.g., digoxin, phenytoin), while in some cases clearance rates decrease (e.g., theophylline).
Teratology is the study of environmentally induced congenital anomalies. A teratogen is an agent, which by acting on the developing embryo or foetus, can cause a structural anomaly. To date, very few drugs are proven teratogens. However, malformations induced by drugs are important because they are potentially preventable.
PRINCIPLES OF TERATOLOGY
Teratogens act with specificity in that they produce specific abnormalities at specific times during gestation. For example, thalidomide produces limb phocomelia, while valproic acid and carbamazepine produce neural tube defects. Other teratogens are associated with recognizable patterns of malformations, for example, phenytoin with foetal hydantoin syndrome and coumarin anticoagulants with foetal warfarin syndrome (see proven teratogenic drugs in humans for description of the above). Teratogenic specificity also applies to species, for example, aspirin and corticosteroids have been found to be teratogenic in mice and rats but appear to be safe in humans. Thalidomide, on the other hand, was not shown to be teratogenic in rats, a tragic fact that resulted in significant human morbidity.
Teratogens may demonstrate a dose-effect relationship. At low doses there can be no effect, at intermediate doses the characteristic pattern of malformations will result, and at high dose the embryo will be killed.
A dose-response may be considered essential in establishing teratogenicity in animals, but is uncommonly demonstrated in sufficient data among humans. A threshold dose is the dosage below which the incidence of adverse effects is not statistically greater than that of controls. With most agents, a dose threshold for teratogenic effects has not been determined; however they are usually well below levels required to cause toxicity in adults.
Teratogens must reach the developing conceptus in sufficient amounts to cause their effects. Large molecules with molecular weights greater than 1,000 do not easily cross the placenta into the embryonic-foetal bloodstream to exert potential teratogenic effect. Other factors influencing the rate and extent of placental transfer of xenobiotics include polarity, lipid solubility and the existence of a specific protein carrier.
TIMING OF EMBRYONIC AND FOETAL DEVELOPMENT
The effect produced by a teratogenic agent depends upon the developmental stage in which the foetus is exposed to the agent. Several important phases in human development are recognized:
- The time from conception until implantation known as the "all or none" period, when insults to the embryo are likely to result in death of the conceptus and miscarriage (or resorption), or in intact survival. At this stage, the embryo is undifferentiated and repair and recovery are possible through multiplication of the still totipotential cells to replace those which have been lost. Exposure of embryos to teratogens during the preimplantation stage usually does not cause congenital malformations, unless the agent persists in the body beyond this period.
- The embryonic period, from 18 to 54-60 days after conception is the period when the basic steps in organogenesis occur. This is the period of maximum sensitivity to teratogenicity since not only are tissues differentiating rapidly but damage to them becomes irreparable. Exposure to teratogenic agents during this period has the greatest likelihood of causing a structural anomaly. Since teratogens are capable of affecting many organ systems, the pattern of anomalies produced depends upon which systems are differentiating at the time of teratogenic exposure.
- The foetal phase, from the end of the embryonic stage to term, is the period when growth and functional maturation of organs and systems already formed occurs. Teratogen exposure in this period will affect foetal growth (e.g., intrauterine growth retardation), the size of a specific organ, or the function of the organ, rather than cause gross structural anomalies. The term foetal toxicity is commonly used to describe such an effect. Of particular interest is the potential effect of psychoactive agents (e.g., antidepressants, antiepileptics, alcohol and other drugs of abuse) on the developing central nervous system, which has led to a new field of behavioural teratology.
Many organ systems continue structural and functional maturation long after birth. Most of the adenocarcinomas associated with first trimester exposure to the synthetic estrogen, diethylstilbestrol, occurred many years after the exposure.
EVALUATION OF DRUGS FOR POTENTIAL TERATOGENICITY IN HUMANS
All new drug applications filed with the United States Food and Drug Administration (FDA) include data from animal developmental and reproductive-toxicologic studies. Although major new teratogenic drugs in humans have been predicted from animal studies, there are problems in extrapolating animal data to humans. Animals have a different "gestational clock" to humans, there is marked interspecies variability in susceptibility to teratogens and no experimental animal is metabolically and physiologically identical to humans. Animal studies are important because, in some instances, they have shed light on mechanisms of teratogenicity and because when an agent causes similar patterns of anomalies in several species, human teratogenesis should also be suspected.
For obvious ethical considerations no studies of teratogenicity are conducted during embryogenesis in humans. The studies are, therefore, either retrospective in nature (case reports, case-series and case-control studies), or prospective cohort studies, where a specific maternal exposure in question is ascertained during pregnancy and the pregnancy outcome is evaluated and compared to a control group. Retrospective case-control studies are less costly and easier to conduct but they have other weaknesses such as the inaccuracy of data collected from medical records and recall bias. For the rare malformation/rare exposure, the case report method is commonly used to suggest association, but case reports are unable to prove or disprove teratogenicity, nor can they give estimation of teratogenic risk. Human teratogenicity is supported by:
- A recognizable pattern of anomalies.
- A statistically higher prevalence of a particular anomaly in patients exposed to an agent than in appropriate controls.
- Presence of the agent during the stage of organogenesis of the affected organ system.
- Decreased incidence of the anomaly in the population prior to the introduction of the agent.
- Production of the anomaly in experimental animals by administering the agent in the critical period of organogenesis.
In an attempt to provide the practitioner who is considering treatment of the pregnant woman with a better assessment of foetal risk, the FDA developed a classification of foetal risk in 1979 (Table 1). The subscript "m" denotes that it is a manufacturer's designation. These categories initially appeared logical, but were not found to be very helpful in counselling individual patients. The manufacturers may have legal rather than scientific reasons for their particular designations. The classification frequently resulted in ambiguity and even in false alarm. For example, the oral contraceptive hormones are denoted as X, despite failure of two meta-analyses to show increased teratogenic risk with their use. The Teratology Society stated in 1994 that the FDA ratings are inappropriate for the purpose of therapeutic guidance to physicians and that the risk of such abuse exceeds the benefits of the system. The Teratology Society recommended that the FDA ratings be deleted from drug labelling and replaced by narrative statements that summarize and interpret available data regarding hazards of developmental toxicity and provide estimates of teratogenic risk. Shepard summarized the criteria for establishing human teratogenicity (Table 2).
TABLE 1 - USE-IN-PREGNANCY RATING (US FDA, '79)
TABLE 2 - AMALGAMATION OF CRITERIA FOR PROOF OF HUMAN TERATOGENICITY*
TERATOGENIC COUNSELLING
In counselling the pregnant patient exposed to a potential human teratogen, it is important to emphasize the significance of exposure to the patient. Ascertaining the clinical facts regarding the nature of the exposure: the length, dosage, and timing of exposure during pregnancy, as well as other exposures of concern about which the patient may not ask (e.g., alcohol, cigarette smoking). All available current data regarding the agent are then collected, and conclusions regarding the risks of exposures are drawn. Counselling should include the background human baseline risk for major malformations, whether the foetus is at increased risk, which anomaly has been associated with the agent in question, a risk assessment, methods of prenatal detection, when available, limitations in our knowledge, and limitations of prenatal diagnostic capabilities. Additional aspects include the potential risk of the medical condition for which a drug is prescribed, known interactions (in both directions) between the disease state and the pregnancy and preventive measures, when applicable (e.g., folic acid supplementation in the case of carbamazepine exposure). Because more than 50% of pregnancies in North America are unplanned, teratogenic risk assessment should be started prior to pregnancy.
PROVEN TERATOGENIC DRUGS IN HUMANS
The foetal alcohol syndrome is a clinical pattern of anomalies characterized by intrauterine growth retardation which commonly continues postnatally. These include: microcephaly, developmental delay, and dysmorphic facies consisting of low nasal bridge, midface hypoplasia, long featureless philtrum, small palpebral fissures and thin upper lip. Cleft palate and cardiac anomalies may also occur. Full expression of this syndrome occurs with chronic daily ingestion of at least 2 grams alcohol per kilogram (eight drinks per day). The full syndrome is present in about one third of these mothers and partial effects occur in approximately three quarters of offspring.
2. Angiotensin converting enzyme inhibitors (ACEI) (captopril, enalapril, lisinopril)
ACEI are potent anti-hypertensive drugs. Their use in late pregnancy has been associated with foetal toxicity including intrauterine renal insufficiency. Reports of neonatal hypotension, oliguria with renal failure, and hyperkalemia have been reported with ACEI use in pregnancy. Complications of oligohydramnios (i.e., foetal limb contractures, lung hypoplasia, and craniofacial anomalies), prematurity, intrauterine growth retardation, and foetal death have also been reported with the use of these agents late in pregnancy. The adverse effects are related to the haemodynamic effects of ACEI on the foetus, teratogenic risk with first trimester exposure to these agents appears to be low.
3. Carbamazepine
Exposure to carbamazepine in utero carries a 1% risk of neural tube defects (10 times their baseline risk). A pattern of malformations similar to those described with the foetal hydantoin syndrome has also been associated with carbamazepine exposure in pregnancy.
4. Cocaine
Cocaine use during pregnancy has been associated with abruptio placentae, prematurity, foetal loss, decreased birth weight, microcephaly, limb defects, urinary tract malformations, and poorer neurodevelopmental performance. The contribution of cocaine to the incidence of congenital malformations is difficult to assess because of methodological problems, which make the results difficult to interpret. Cocaine abuse is often associated with poly-drug abuse, alcohol consumption, smoking, malnutrition, and poor prenatal care. Experimental animal studies and human epidemiology indicate that the risk of major malformation from cocaine is probably low, but the anomalies may be severe.
5. Coumarin anticoagulants
First trimester exposure to coumarin derivatives is associated with a characteristic pattern of malformations termed the foetal warfarin syndrome. Clinical features consist of nasal hypoplasia and calcific stippling of the epiphyses. Intrauterine growth retardation and developmental delay due to central nervous system damage, eye defects, and hearing loss have also been described. The critical period of exposure for the foetal warfarin syndrome appears to be between 6 and 9 weeks of gestation. A prospective study found evidence of warfarin embryopathy in about one third of the cases where a coumarin derivative was given throughout pregnancy. Oral anticoagulants are also associated with a high rate of miscarriage. Exposure to oral anticoagulants after the first trimester presents a risk of central nervous system damage due to haemorrhage. Unlike heparin, oral anticoagulants readily cross the placental barrier.
6. Diethylstilbestrol
Diethylstilbestrol was used in the 1950s and 1960s for the diagnosis of recurrent miscarriage. Clear cell adenocarcinoma of the vagina was found to be associated with diethylstilbestrol treatment of the patient's mother during the first trimester of pregnancy. Over 90% of the cancers occurred after 14 years of age. Clear cell carcinoma has not occurred in women exposed in utero after the 18th week of gestation. A high incidence of benign adenosis of the vagina was found in women prenatally exposed to this nonsteroidal estrogen analogue. In a prospective study, exposure starting at 4 weeks was associated with adenosis in 56% of the offspring, decreasing later to 30% at 16 weeks and 10% at 20 weeks. Miscarriage rate and preterm delivery were significantly more common in women exposed in utero to diethylstilbestrol compared to matched controls. In 134 males exposed in utero to the agent no signs of malignancy were found but 27% had genital lesions (epididymal cysts, hypotrophic testes, or capsular induration of the testes). In 29%, pathologic changes were found in spermatozoa.
7. Folic acid antagonists: Aminopterin and methotrexate
Aminopterin has been known since 1950 to result in foetal death, which led to its use as a human abortifacient. The foetal aminopterin syndrome was described based on anomalies observed in aborted foetuses and infants born following unsuccessful abortions. Malformations include central nervous system defects (hydrocephalus, meningomyelocele), facial anomalies (cleft palate, high arched palate, micrognathia, ocular hypertelorism, external ear anomalies), abnormal cranial ossification, abnormalities in first branchial arch derivatives, intrauterine growth retardation and mental retardation. Infants have been born with features of the aminopterin syndrome after pregnancy exposure to methotrexate (methylaminopterin). It was suggested that the maternal dose necessary to induce defects is above 10 mg per week with a critical period of 6 to 8 weeks post conception being postulated.
8. Hydantoins (phenytoin and trimethadione)
Hydantoins have been associated with a recognizable pattern of malformation termed the foetal hydantoin syndrome. The clinical features include craniofacial dysmorphology (wide anterior fontanelle, ocular hypertelorism, metopic ridge, broad depressed nasal bridge, short anteverted nose, bowed upper lip, cleft lip, cleft palate), as well as variable degrees of hypoplasia of the distal phalanges, nail hypoplasia and low arch dermal ridge patterning. Growth retardation, mental deficiency and cardiac defects are additional features of the syndrome.
9.Isotretinoin (13-cis-retinoic acid)
Isotretinoin is a synthetic vitamin A derivative, prescribed for severe cystic acne, that has been proven to be a potent human teratogen as well as a behavioural teratogen when given systemically. A pattern of anomalies termed retinoic acid embryopathy has been associated with isotretinoin (and other retinoic acid derivatives such as etretinate and megadoses of vitamin A) exposure in pregnancy. The clinical features include craniofacial anomalies (microtia or anotia, accessory parietal sutures, narrow sloping forehead, micrognathia, flat nasal bridge, cleft lip and palate, and ocular hypertelorism), cardiac defects (primarily conotruncal malformations), abnormalities in thymic development, and alterations in central nervous system development. The risk for associated miscarriage was 40%.
10. Lithium
By 1983, the International Registry of Lithium Babies had collected retrospective information on 225 babies exposed to lithium during the first trimester. Despite the lack of a control group and the likely over-reporting of abnormal outcome, the data suggested a higher risk for major anomalies than in the general population and a specific risk for cardiac teratogenesis in early gestation. The number of cases of Ebstein's anomaly, a rare malformation of the tricuspid valve, by far exceeded its spontaneous rate of occurrence. In a prospective study of 148 women who took lithium during the first trimester of pregnancy, three infants were born with major malformations, a rate comparable to that found in the control group. One pregnancy was terminated following prenatal diagnosis of Ebstein's anomaly. Foetal echocardiography is recommended in the management of pregnancies exposed to lithium in the first trimester.
Misoprostol is a synthetic prostaglandin E1 analogue, prescribed for duodenal and gastric ulceration, also used as an abortifacient by women in Brazil. A Brazilian case-series suggested an association between first trimester exposure to misoprostol and limb defects with or without Moebius' sequence. The association was further supported by a case-control study comparing the frequency of misoprostol use during the first trimester by mothers of 96 infants with Moebius' syndrome and mothers of infants with neural tube defects. Among the mothers of infants with Moebius' syndrome, 49% had used misoprostol, as compared with 3% of the mothers of infants with neural tube defects (odds ratio, 29.7; 95% confidence interval 11.6 to 76.0). Despite the strong association between misoprostol exposure during the first trimester and Moebius' syndrome, its absolute teratogenic risk is probably not high.
12. Tetracyclines
Yellow-brown discolouration of teeth may occur due to deposition of the antibiotic in calcifying teeth with tetracycline use in late pregnancy. The risk is apparent only after 17 weeks of gestation when the deciduous teeth begin to calcify. Generally, only the deciduous teeth are involved, although with administration of the drug close to term the crowns of the permanent teeth may be stained. Oxytetracycline and doxycycline are associated with a lower incidence of enamel staining.
More than any other event, the thalidomide tragedy alerted the world to the teratogenic potential of drugs. Thalidomide was marketed in 1956 and was available for four years before its teratogenicity was recognized. Thalidomide produced malformations limited to tissues of mesodermal origin, primarily limbs, ears, cardiovascular system, and gut musculature. The types of malformations could be related to the developmental stage of the embryo at the time of ingestion. Malformations resulted from repeated use as well as from single ingestions during the critical period from the 27th day to the 40th day of gestation. In women, a single dose of less than 1 milligram per kilogram has produced the syndrome. Abnormal development of long bones produced a variety of limb reduction defects. Typically the upper limbs were more severely involved than the lower limbs. However, any of the bones could be defective or, in severe cases, totally absent. Phocomelia, polydactyly, syndactyly, oligodactyly were all reported. Lower extremities could be similarly affected, although less frequently and less severely. Defects of the external ears ranging from agenesis to preauricular tags occurred in 20% of cases and were the earliest of the recognized thalidomide anomalies. Other anomalies associated with phocomelia are facial capillary haemangiomas, and palsies of cranial nerves VI or VII. A wide variety of cardiovascular defects were seen, affecting about 10% of infants. Visceral anomalies included agenesis of kidneys, spleen, gallbladder and appendix and atresias or stenoses of the esophagus, duodenum, and anus. Cleft palate was a rare complication and the central nervous system was not adversely affected as reflected by normal intelligence. It has been estimated that the embryopathy was found in about 20% of the pregnancies with exposure to thalidomide in the critical period.
14. Valproate
First trimester exposure to valproate is associated with neural tube defects and carries a 1-2% risk of meningomyelocele, primarily lumbar or lumbosacral. A number of investigators have delineated an associated pattern of malformations, which they termed the foetal valproate syndrome. The clinical features include narrow bifrontal diameter, high forehead, epicanthal folds, infra-orbital creases, telecanthus, low nasal bridge, short nose with anteverted nares, midfacial hypoplasia, long philtrum, thin vermillion border, small mouth, cardiovascular defects, long fingers and toes, hyperconvex fingernails, and cleft lip.
POSSIBLE TERATOGENIC DRUGS IN HUMANS
D-penicillamine
Based on several case reports, high dose treatment of the pregnant woman with D-penicillamine has been associated with connective tissue disorders (cutis laxa).
Methimazole
Methimazole treatment during pregnancy has been associated with scalp defects (aplasia cutis congenita) based on case reports and on an epidemiological study in which methimazole had been added to animal feeds as a weight enhancer, and in those areas a higher incidence of cutis aplasia congenita was found.
Diazepam
First trimester exposure to diazepam has been associated in small studies with a small increase in the incidence of cleft lip and palate. Larger studies did not confirm the association.
Subscribe to:
Posts (Atom)